In search of new ways to target lung cancer cells, researchers in this study demonstrated that miR-708 has anti-tumorigenic properties.
The Trending with Impact series highlights Oncotarget publications attracting higher visibility among readers around the world online, in the news, and on social media—beyond normal readership levels. Look for future science news and articles about the latest trending publications here, and at Oncotarget.com.
—
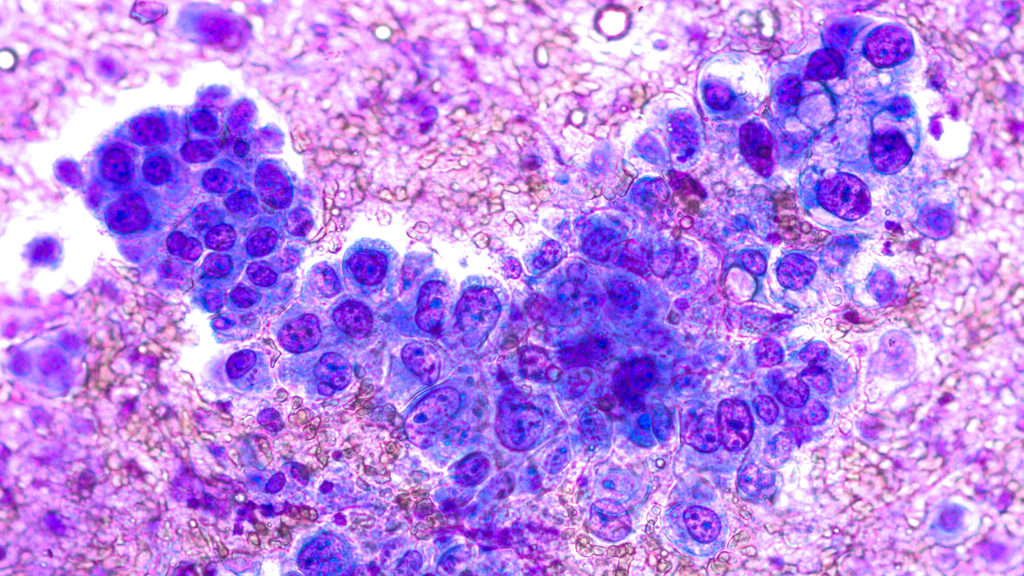
Despite the innumerable biomedical advancements made in the detection, classification, and treatment of cancer since the 1971 National Cancer Act, lung cancer survival rates are still staggeringly low. In addition, every year over $12.1 billion is spent on lung cancer care in the United States. Non-small cell lung cancer (NSCLC) contributes to 85% of lung cancers, and within this classification there are two main subtypes: adenocarcinoma (LUAD) and squamous cell carcinoma (LUSC).
“Although tumors are differentiated by subtype, LUAD and LUSC are generally treated with the same chemotherapeutics.”
Researchers, from the New Jersey Medical School’s academic health center, Rutgers Biomedical & Health Sciences, say that discovering new biomarkers that can help better distinguish between NSCLC subtypes is necessary to improve patient outcomes. In 2020, they conducted a study of a microRNA that is dysregulated in lung cancer, miR-708, to clarify its tumor suppressive or oncogenic functions within lung cancer cells.
“Lung cancer is a complex collection of deadly diseases that are generally hard to detect and treat. Therefore, it is crucial to develop novel methods to identify, distinguish, and treat lung cancer.”
The Study
The researchers in this study explain that it is crucial to take the entire tumor microenvironment (TME) into consideration when devising treatments for cancerous tumors. Historically, many chemotherapies that have been developed are successful in targeting tumors, but contribute to damaging the surrounding cells and tissues in the TME—contributing to harm and extending recovery time. In newer treatments being developed, researchers have considered the benefits of targeting the pro-tumor effects of particular immune cells and activating the immune system to attack cancer cells.
“miR-708 has previously been described as being both oncogenic and tumor suppressive in lung cancer [63–65]. Therefore, we aimed to clarify the tumor suppressive or oncogenic functions of miR-708 in lung cancer cells.”
To determine the clinical relevance of miR-708 in lung cancer patients, the researchers analyzed data from The Cancer Genome Atlas (TCGA) using the TCGA-assembler 2 R software package. They used mammalian cell cultures to perform miRNA and 5-Azacytidine treatments, RNA isolation using TRIzol, quantitative real-time RT-PCR, western blot analysis, plasmids, luciferase reporter assays, Enzyme-Linked Immunosorbent Assay (ELISA) analysis, phenotypic assays; Water Soluble Tetrazolium Salts (WST)-1 assay; Ki-67 staining; Annexin V staining; Cell migration assay, and Bioinformatic and statistical analyses.
“We next examined expression of miR-708 in normal and lung cancer cells to determine if our cell lines faithfully replicated clinical data.”
Results
The researchers demonstrated that miR-708 was underexpressed in lung cancer cells compared to normal lung cells. A lower expression of miR-708 correlated with decreased survival in patients with squamous cell carcinoma non-small cell lung cancer. They demonstrated that miR-708 suppressed the production of the pro-tumorigenic hormone called prostaglandin E2 (PGE2) (located in the arachidonic acid (AA) metabolic inflammatory pathway), by directly repressing the expression of COX-2 and mPGES-1 in lung cancer cells.
“We also demonstrated that miR-708 decreases lung cancer cell metabolism (Figure 5), proliferation (Figure 6), survival (Figure 7), and migration (Figure 8).”
Conclusion
The researchers were left with some outstanding questions about miR-708. First, they wondered why miR-708 expression is decreased in lung cancer cells compared to normal cells in the lungs. They suggest the cause may be the hypermethylation of the ODZ4 promoter region in lung cancer cells, a loss of tumor suppressive transcription factors, repressed CHOP activity, or specifically, the glucocorticoid receptor-alpha (GRα) repression of CHOP activity.
“Our work has identified novel tumor suppressive miR-708 functions by suppressing oncogenic PGE2 production through targeting of COX-2 and mPGES-1. These findings could be the foundation for identifying novel miR-708 targets, as well as regulators of miR-708 expression in cancer.”
“Moreover, our study highlights the need to better understand lung cancer biology to improve diagnosis and treatment of lung cancer, ultimately aiming to increase positive patient outcomes.”
Click here to read the full scientific study, published in Oncotarget.
Visit Oncotarget.com for the Special Collection on Lung Cancer
—
Oncotarget is a unique platform designed to house scientific studies in a journal format that is available for anyone to read—without a paywall making access more difficult. This means information that has the potential to benefit our societies from the inside out can be shared with friends, neighbors, colleagues, and other researchers, far and wide.
For media inquiries, please contact media@impactjournals.com.