Researchers developed a nanoparticle-based T cell engager (nanoTCE) technology believed to be capable of targeting any immune cell and cancer of interest. NanoTCE efficacy was examined in acute myeloid leukemia.
Picture the human body’s immune response as analogous to the action of an army of military soldiers. For the most part, a healthy immune system can “hold down the fort” and protect the body from many perils of the outside world. We often rely on our immune system’s discretion to determine when and which invaders our soldiers (T cells, for example) should attack. However, when it comes to fighting the most dangerous and formidable opponents, including cancer, researchers have invested in developing new immunotherapies to help boost the body’s own immune response.
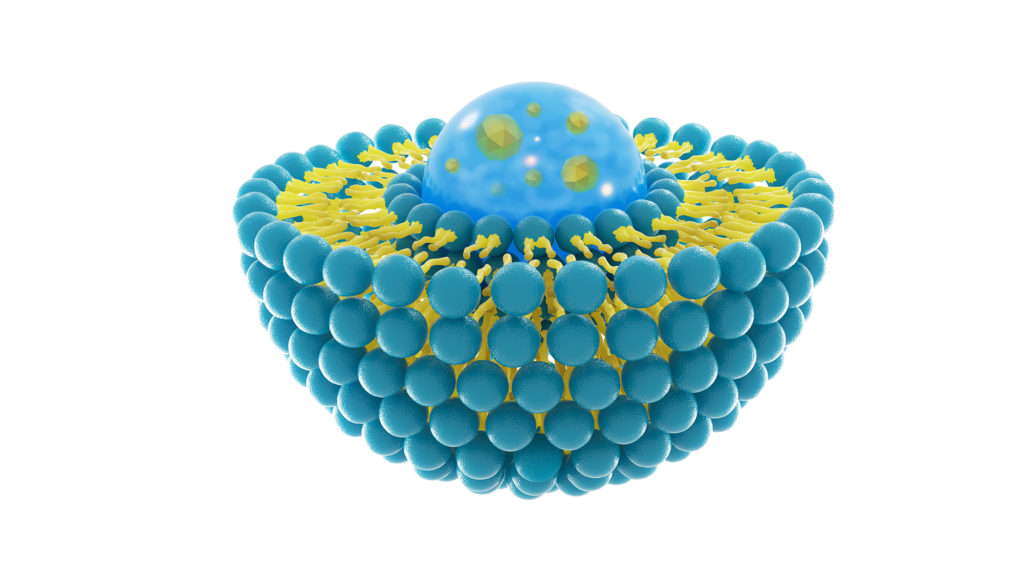
One method of immunotherapy drug delivery is liposomal nanoparticles. Natural liposomes are spherical sacs that contain phospholipids; liposomes can also be formed artificially to carry drugs and other substances into tissues. A new immunotherapy technology using liposomal nanoparticles was recently developed, called a nanoparticle-based T cell engager (nanoTCE).
“We have previously developed a nanoparticle-based T cell engagers (nanoTCEs) technology that is based on conjugation of two monoclonal antibodies (mAbs) to the surface of a liposomal nanoparticle; one antibody is against a cancer antigen and the other is against the CD3 receptor on T cells [16].”
The nanoTCE is a highly customizable technology that combines T cell activation with targeted cancer therapy. Researchers, from Washington University School of Medicine and Washington University McKelvey School of Engineering, claim that this highly specific technology can be engineered to engage with any immune cell to target and treat any cancer of interest. The team conducted a study using the nanoTCE technology in the treatment of acute myeloid leukemia (AML). Their paper was published on the cover of Oncotarget’s Volume 12, Issue 19, and entitled, “Nanoparticle T cell engagers for the treatment of acute myeloid leukemia.”
The Study
In this study, the team conducted in vitro and in vivo experiments using cell cultures and murine models of four different human AML cell lines, the nanoTCE technology, immunotherapies, and controls. Since the protein coding gene CD33 is well-known to be highly expressed in AML—found on as much as 85–90% of blasts—the researchers used CD33 as a targetable biomarker for AML immunotherapy.
“CD33 is a valuable target for the treatment of AML, therefore, we first validated the presence of the marker in our experimental setup.”
Next, researchers designed a nanoTCE domain to recognize a CD33 tumor-associated surface antigen and the other domain to recognize the T cell CD3 receptor (to activate T cell response). In addition to the in vitro experiments, murine models of AML were administered weekly doses of CD33/CD3 nanoTCEs. In vitro, study results demonstrated that CD33/CD3 nanoTCEs preferentially bound to AML cells when compared to the isotypes. They also found that in vivo AML models treated with CD33/CD3 nanoTCEs had significantly lower tumor burden at all time points compared to the controls.
“The CD33 nanoTCEs bind preferentially to AML cells compared to Isotype. We show that nanoTCEs effectively activate T cells and induce AML killing in vitro and in vivo.”
Conclusion
“In this study, we report a CD33/CD3 nanoTCE that targets the CD33 antigen with high specificity using mAbs, which enables a potent and efficacious immunotherapy treatment against AML. Future studies are warranted to investigate this therapy in combination with chemotherapy, the extent this technology eliminates minimal residual disease and relapse, as well as its efficacy in AML patients.”
Click here to read the full research paper, published by Oncotarget.
YOU MAY ALSO LIKE: More Oncotarget Videos on LabTube
—
Oncotarget is a unique platform designed to house scientific studies in a journal format that is available for anyone to read—without a paywall making access more difficult. This means information that has the potential to benefit our societies from the inside out can be shared with friends, neighbors, colleagues, and other researchers, far and wide.
For media inquiries, please contact media@impactjournals.com.