Dr. Beatrice Aramini and Dr. Valentina Masciale provide an overview of their cancer research published in Oncotarget, titled: “Cancer stem cells and macrophages: molecular connections and future perspectives against cancer.”

The Behind the Study series transcribes videos of chosen researchers elaborating on their recent papers published in Oncotarget. Visit the Oncotarget YouTube channel for more insights from outstanding authors.
—
Good morning. I’m Dr. Beatrice Aramini. I’m a thoracic surgeon and scientist. I mainly focus on lung cancer. I started this project about cancer stem cells in lung cancer since 2017, at University Hospital of Modena Reggio Emilia, joining the laboratory of cell therapies directed by Professor Massimo Dominici with the Chief of Medical Oncology at University Hospital in Modena.
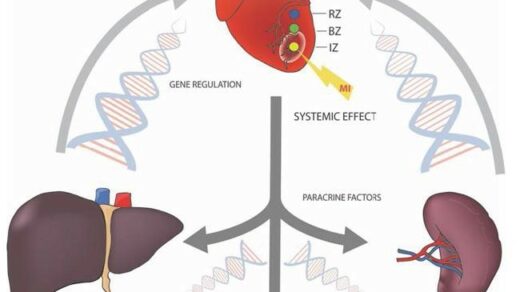
With this interview, we would like to show the main points of this review article entitled, “Cancer stem cells and macrophages, molecular connection and future perspectives against cancer” already accepted by Oncotarget Journal. In this review, we describe the importance of cancer stem cells as the key drivers of cancer initiation and progression due to their unlimited cell renewal capacity and their ability to induce tumor formation. Macrophages, particularly tumor associated macrophages, establish a tumor microenvironment to protect and induce cancer stem cells’ development and dissemination. Many studies in the past decade have been performed to understand the molecular mediators of cancer stem cells and tumor-associated macrophages. And several studies have elucidated the complex crosstalk that occurs between these two cell types.
The aim of this review is to define the complex crosstalk between these two cell types and to highlight potential future anti-cancer strategies. Cancer stem cells constitute a cancer cell subpopulation similar to the other stem cell types in terms of self-renewal and multi-lineage differentiation potential, but drive tumor development besides heterogeneity and dissemination of cancer cells. Cancer stem cells have been extensively studied with some of these studies focusing on their identification and their origin from differentiated cancer cells due to macro environment influence, which contributes to their heterogeneous phenotypes.
Targeting cancer stem cells for therapeutic purposes is a goal of the scientific community. Currently, cancer treatments target the bad population of the tumor cells without identifying and targeting cancer stem cells. One of the major problems in finding such a marker is that several markers are able to detect not only cancer stem cells but also non-tumor cells, which represents an obstacle in developing new therapies targeting cancer stem cells.
Most of the markers identifying stem cells are proteins or lipoproteins, and these identification markers may be subjected to genetic modifications. Another sensor characteristic of these markers is the variability in their localization as they may be on the cell membrane or into the cytoplasma as, for example, genesis 1, which is located in the cytoplasma and has been observed in several solid tumors, as well as in leukemia.
The localization and the characteristics of these markers reveal that cancer stem cells may have different epigenetic and genetic alterations. This may be one of the most important reason why scientists are still debating about possible cancer stem cells markers in different solid tumors. Despite that, this aspect has been investigated in cells line and experimental model animal for decades. However, currently there is no specific or standard market in lung cancer cells that can be defined. These two populations of cells are probably due to the complex localization of these markers and their epigenetic regulation.
Different markers for cancer stem cells have been studied in the last recent decades and scientists try to attempt to improve identification of this super population by using a double or triple marker, our group, but at Barton, another super population of cells expressing CD 44 positive, outcome positive cells that were positively correlated with LDH positive cells. We compare to similar cancers, their population, and this significant data may form the basis to develop new target treatments, to eliminate cancer stem cells, which are considered to be one of the leading causes of tumor recurrence and progression the complexity of cell composition, which is the base of cancer heterogeneity has been discussed for a long time due to the different mechanism at the top, the cause of the consumerization process. Learnability moreover the discovery of the plasticity of cancer stem cells and the possibility of switching from stem to non stem cells led to a more complex picture of the origin of tumor heterogeneity.

Although the cancer stem cell model alone is not support enough to explain functional heterogeneity in cancer, scientists have recently considered the role of the tumor marker environment, has it significant factor in cancer stem cells plasticity, especially in the process of turning from non-cancer stem cells to cancer stem cells. And this mechanism seems to rely on cell to cell interactions within the tumor niche. Furthermore, the disconnections between cancer stem cells and other cells is the primary source of protection for this super population during induction of cell transformation to grow more resistant to common oncological treatments.
In this context that the tumor micro environment seems to play a crucial role in tumor progression and metastasis by building a synergistic relationship with cancer stem cells. I would like to introduce Dr. Valentina Masciale who’s a research fellow at university hospital. Her professional experience started firstly, on the study of missing stroma cells, then stem cells in a regenerative medicine, and now she’s involved with me in a project focused on lung cancer stem cells. She will describe the main biological points of this review.
Dr. Valentina Masciale
Good morning to everyone. As Dr. Aramini just said the role of cancer stem cell in carcinogenesis has not yet been well-defined, even if it is actually known that involvement as key driver of tumor initiation progression and metastatic process. In particular, the contribution of the tumor microenvironment in the metastatic process is important as it provides favorable signal to support the metastatic cascade, especially through tumor-associated macrophages. They comprise up to 50% of the tumor mass divided into two principal subtype, the M1 microphages expressing CD 68, which are mainly involved in inflammatory activities and M2 microphages expressing the CD 163, which promote anti-inflammatory processes.
The rising interest on these type of cells comes from recent study demonstrating that high number of tumor-associated microphages correlate with the poor clinical prognosis in many solid tumors, including lung cancer, which is the field of our research group at the University Hospital of Modena. Another important aspect is the protective role of the tumor-associated microphages play on tumors undergoing chemotherapy, which may impact the chemotherapy resistance and consequent tumor relapse.
Recently, it has been demonstrated that tumor-associated macrophages in breast cancer are responsible for chemotherapy drug resistant through different signaling pathways, like as the interleukin 10 state three BCL 2, and also for favorable outcomes during radiotherapy due to their capacity to modulate the cancer cells response to therapy. These explain the great interest on the scientific community in exploring target therapies against tumor-associated microphages to improve the efficacy of therapy and chemotherapy.
In particular, the inhibition of tumor associated macrophages recruitment can prevent tumor growth. In this review article, we also explain the involvement of the immune process in the control of tumor progression we describe, the immuno processes that lead to control of the tumor progression, including the important phase of the immunosurveillance in which cancer stem cells are able to escape the immune system through. For example, the downregulation of the antigen presenting cells, the antigen processing machinery is the effect in cancer stem cell that these highly specialized stents exhibit low immunogenicity. Some cancer stem cells, particularly melanoma modulate immune response by expressing ABCB five gene comparing chemo resistance.
These mechanisms mentioned, are responsible for the modulation of the immune response through the induction of T-cell anergy and downregulation of cancer associated antigens to escape immunity, to more players. Another mechanism that can influence immune cell presence and function is associated with tumor associated microphages. Tumor associated microphages are the predominant immune cells within tumors, consequently, they significantly impact the tumor initiation process and can affect the T lymphocytes natural killer cells, dendritic cells, neutrophils, and myeloid derived suppressor cells.
Also tumor-associated macrophages express two markings like CCL5, CCL22 CCL20 and cytokines like interleukin 10 TGF B which record with an activate regulatory T cells thus contributing to the immunosuppression, the tumor microenvironment, and participate in tumor cell escape and tumorigenesis, in particular tumor associated macrophages can surprise the antitumor effect of tumor-infiltrating T-cells NK cells and any meat. The cell function by releasing a specific enzyme such as nitric, oxide synthase, and arginase one. Besides tumor associated macrophages suppresses cytotoxic function of these cells lymphocytes the true expression of the ligands for PD one and CTLA four immunotherapies to fight cancer such as checkpoint inhibitors or lymphocyte transplant strategies are managing novel therapeutic approaches in the oncology field.
Dr. Beatrice Aramini
With regard of the future perspective in cancer, surgery is nowadays considered the gold standard treatment that only for cancer in early stages and locally advanced stages, whereas treatment of advanced cancer stages required chemotherapy and radiotherapy alone or in combination. However, in many cases, all treatments, chemo, radio and immunotherapy fail to prevent cancer recurrence. The primary cause of failure in cancer treatment is the emergence of drug resistance that promotes the tumor spreading. Several investigated the best cell target to fight cancer, including, but not limited to two cancer stem cells since cancer stem cells are sustained by other cells, including tumor associated macrophages. Another approach recently taken into consideration as a prospective approach in cancer therapies, is nanomedicine. The cell base, the target nanoparticles have been described in several studies and kind of geared toward antibodies and died and so on.
The most complicated aspect of this interaction, that is the space between the target and the moleculars that needs to be bound. This is space must be not larger than a few nanometers, otherwise, the interaction would not be effective. This aspect is easy to address in vitro, but it may represent the problem in vivo as the characteristic of tumor, microenvironment are more varied and are different from the media commonly used in vitro. It has been shown that the target of nanoparticles does not produce an increment of these particles, able to buy cancer cells in vivo.
This aspect is suggested that the target of cell based non particles in ecology has been over considered while the physical characteristics of nano particle must receive more focus. In addition to this aspect, that the macro environment, particularly the cell to cell interaction and the cell immune system interactions should also be taken into consideration as they may constitute a huge stock for the optimization of this across against cancer, the synthesis of oral nano drugs, so will likely be more useful than intravenous solutions and this may represent the main factor in the clinical use of nano drugs to treat cancer.
However, several barriers are required before interaction between the particles and the components of tumor microenvironment. Interestingly, the increasing phagocytic activity of macrophages has been exploited to load anti-cancer nano drugs. One of the first accepted therapies in this field involve the Nova team, delivery of bioactive proteins into macrophages to treat the nature of the genetic diseases. This therapeutic approach is based on, nanozyme which can be rapidly internalized by monocyte derived macrophages, and released in an acting form within 24 hours.
So, in conclusion, understanding the interaction between cancer and cancer stem cells is needed to develop novel treatment strategies in the future. So our review would represent a good start point to refresh, update, and I like the main connection and future perspectives between tumor associated macrophages and cancer stem cell.
—
Oncotarget is a unique platform designed to house scientific studies in a journal format that is available for anyone to read—without a paywall making access more difficult. This means information that has the potential to benefit our societies from the inside out can be shared with friends, neighbors, colleagues and other researchers, far and wide.
For media inquiries, please contact media@impactjournals.com.