Researchers conducted a study to examine the efficacy of adding the P10s-PADRE vaccine to chemotherapy treatments for patients with HR+/HER2− breast cancer.
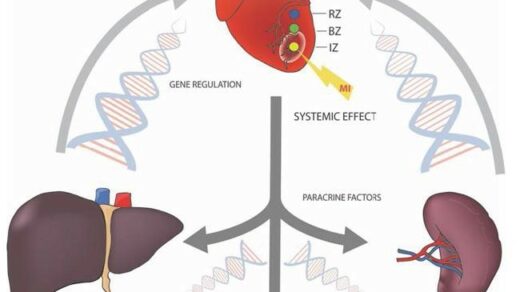
The most common type of breast cancer in the United States is HR+/HER2− breast cancer. Patients with HR+/HER2− breast cancer often face the threat of distant recurrence—long after the completion of their treatment. Previous studies have found that high levels of tumor infiltrating lymphocytes (TILs) were associated with improved outcomes and recurrence-free survival in patients with HR+/HER2− breast cancer. These studies, and many others, have prompted researchers to further develop and test cancer vaccines in an effort to elicit anti-tumor immune responses in these patients.
“Therefore, a rational combination therapy that enhances the immune-stimulatory properties of NAC [neoadjuvant chemotherapy], can provide long-term survival benefits for this patient population.”
Researchers from the University of Arkansas for Medical Sciences, University of Texas Southwestern, Highlands Oncology Group, and Université Claude Bernard Lyon 1 conducted a new single-arm Phase Ib clinical trial. Early-stage HR+/HER2− breast cancer patients were treated with carbohydrate-mimetic peptides, the P10s-PADRE vaccine, in combination with chemotherapy treatments. Their paper was chosen as the cover of Oncotarget’s Volume 12, Issue 22, and entitled, “P10s-PADRE vaccine combined with neoadjuvant chemotherapy in ER-positive breast cancer patients induces humoral and cellular immune responses.”
“The main objective of our study was to determine an appropriate schedule to be used for adding the P10s-PADRE vaccine to cancer chemotherapy in the neoadjuvant setting considering the ability of the vaccine to elicit adequate antibody response.”
The Study
After meeting the study’s detailed inclusion/exclusion criteria, a total of 25 patients with HR+/HER2− breast cancer were selected to partake in this single-arm Phase Ib clinical trial. Patients were divided into five cohorts (five patients per cohort): A, B, C, D, and E. Each patient was treated with a combination of four therapies over the course of 22-25 weeks, including three doses of the peptide-based P10s-PADRE cancer vaccine, four doses of Cyclophosphamide (chemotherapy), four doses of Doxorubicin (chemotherapy) and four doses of Docetaxel (chemotherapy). Using a cohort-specific treatment schedule for the previously stated combination of therapies, the researchers assessed the feasibility, safety and immunogenicity achieved in each cohort and each patient.
Additionally, patients underwent surgery between weeks 26 and 33 (four to eight weeks after their last chemotherapy treatment). Each cohort also had a cohort-specific blood draw schedule—blood was drawn at eight different times in the 73-week time frame. Blood draws were used to conduct flow cytometry, measure the concentration of cytokines, natural killer (NK) cells and antibodies, and to determine the presence of anti-peptide antibody response and the percentage of TILs. The researchers observed that all five cohorts saw a significant reduction in tumor size.
“The data suggest that subjects enrolled in schedule C generated a more consistent and robust antibody response, therefore schedule C appears as the schedule of choice for future combination therapy.”
Their findings concluded that, in combination with chemotherapy, P10s-PADRE immunization in HR+/HER2− breast cancer patients induced “acceptable” antibody responses in study cohorts C and E. The treatment schedule in cohort C demonstrated the strongest antibody response by affecting the expression levels of NK-cell markers, stimulating the production of cytokines, T-cells and TILs. However, the researchers note that continued analysis of the blood samples collected could show serum antibodies may begin to appear later on in patients enrolled in the other treatment schedules.
Conclusion
“This Phase Ib clinical trial of the P10s-PADRE vaccine shows that immunization in combination with a standard-of-care NAC is feasible and well-tolerated. Combination therapy induces antibody response, stimulates activation of NK cells, and is associated with infiltration of T cells in tumor microenvironment. Randomized phase II trials focusing on treatment schedule C are needed to validate current findings and evaluate clinical efficacy.”
Click here to read the full research paper, published by Oncotarget.
YOU MAY ALSO LIKE: More Oncotarget Videos on LabTube
—
Oncotarget is a unique platform designed to house scientific studies in a journal format that is available for anyone to read—without a paywall making access more difficult. This means information that has the potential to benefit our societies from the inside out can be shared with friends, neighbors, colleagues, and other researchers, far and wide.
For media inquiries, please contact media@impactjournals.com.